Decoding the Timeline: New CPT Code Application Process Explained
Navigating the complexities of medical coding can be daunting, especially when dealing with Current Procedural Terminology (CPT) codes. These codes are crucial for billing and reimbursement in the healthcare industry. Understanding the timeline new CPT code application process is essential for healthcare providers, administrators, and developers of new medical procedures and technologies. This article provides a comprehensive overview of the application timeline, key milestones, and factors that influence the approval of new CPT codes.
What are CPT Codes and Why Are They Important?
CPT codes are a standardized set of codes developed and maintained by the American Medical Association (AMA). They are used to report medical, surgical, and diagnostic procedures and services to payers, such as insurance companies and government healthcare programs. Accurate and appropriate CPT coding is vital for several reasons:
- Reimbursement: CPT codes form the basis for billing and reimbursement. Incorrect or missing codes can lead to claim denials or underpayment.
- Data Analysis: CPT codes are used to track healthcare trends, utilization patterns, and the effectiveness of different medical interventions.
- Compliance: Proper CPT coding ensures compliance with regulations and guidelines set by payers and regulatory agencies.
The Need for New CPT Codes
The healthcare landscape is constantly evolving, with new medical technologies, procedures, and services emerging regularly. As these innovations become more prevalent, there is a need to create new CPT codes to accurately reflect the work performed. This ensures that providers are appropriately compensated for their services and that data is collected accurately for analysis and research purposes. The timeline new CPT code application process is in place to address this evolving need.
Initiating the New CPT Code Application Process
The process of applying for a new CPT code is rigorous and requires careful preparation. The first step involves identifying a need for a new code. This typically arises when an existing CPT code does not accurately describe a new procedure or service. The applicant, often a physician, medical society, or device manufacturer, must then gather supporting documentation to demonstrate the clinical validity and utility of the new procedure.
Pre-Application Considerations
Before formally submitting an application, several pre-application considerations should be addressed:
- Clinical Evidence: Gather robust clinical evidence, including peer-reviewed publications, clinical trial data, and case studies, to support the safety and efficacy of the new procedure.
- Coding Analysis: Analyze existing CPT codes to determine if any adequately describe the new procedure. If not, clearly articulate why a new code is necessary.
- Market Analysis: Assess the potential impact of the new code on healthcare utilization and costs. Payers will want to understand the potential financial implications.
The Formal Application Submission
Once the pre-application considerations have been addressed, the applicant can proceed with the formal submission. The application must be submitted to the AMA CPT Editorial Panel, which is responsible for reviewing and approving new CPT codes. The application requires detailed information about the procedure, including a description of the technique, indications for use, and expected outcomes. Understanding the timeline new CPT code application is crucial at this stage to manage expectations and allocate resources effectively.
Key Components of the Application
A successful CPT code application should include the following key components:
- Detailed Procedure Description: Provide a comprehensive description of the procedure, including the steps involved, equipment used, and any unique aspects.
- Clinical Rationale: Explain the clinical rationale for the procedure, including the conditions it treats and the potential benefits for patients.
- Clinical Evidence: Present robust clinical evidence, including peer-reviewed publications, clinical trial data, and case studies, to support the safety and efficacy of the procedure.
- Coding Justification: Clearly justify why a new CPT code is needed, explaining why existing codes are inadequate.
- Impact Analysis: Assess the potential impact of the new code on healthcare utilization and costs.
The CPT Editorial Panel Review Process
After the application is submitted, it undergoes a rigorous review process by the CPT Editorial Panel. This panel consists of physicians, healthcare professionals, and coding experts who evaluate the application based on several criteria, including clinical validity, utility, and impact on healthcare costs. The timeline new CPT code application includes several stages of review and deliberation by the panel.
Stages of the Review Process
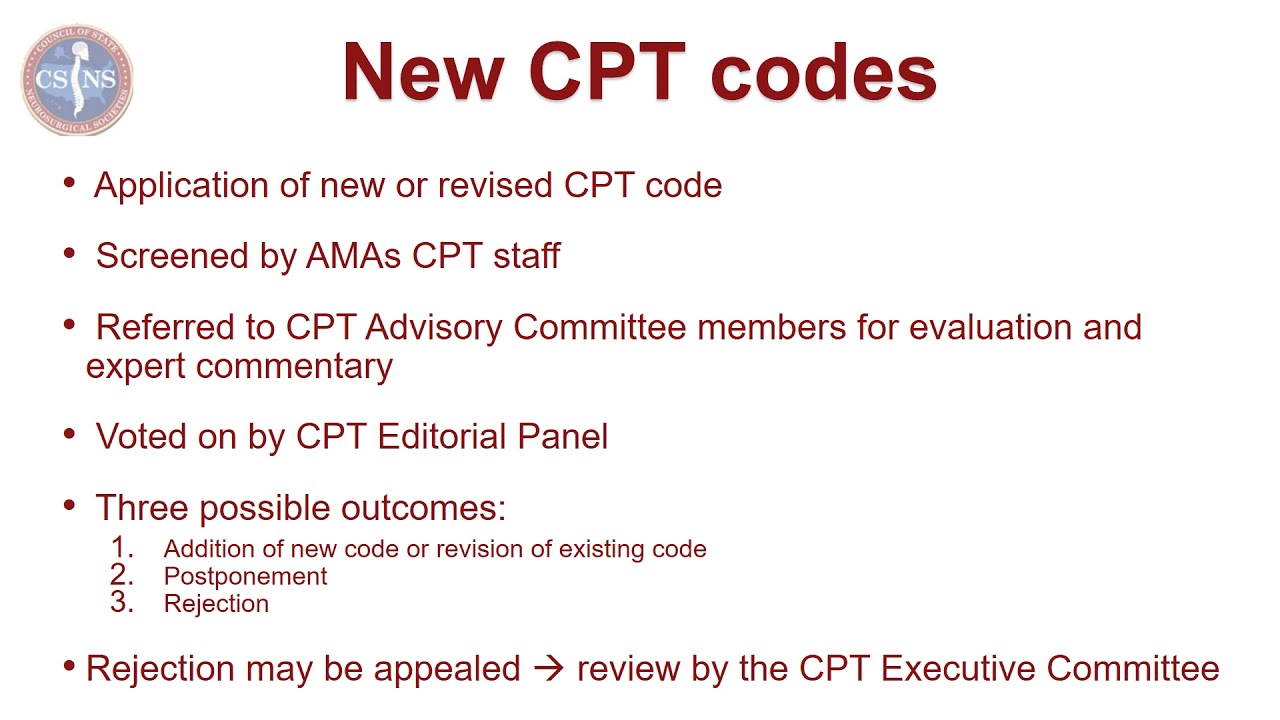
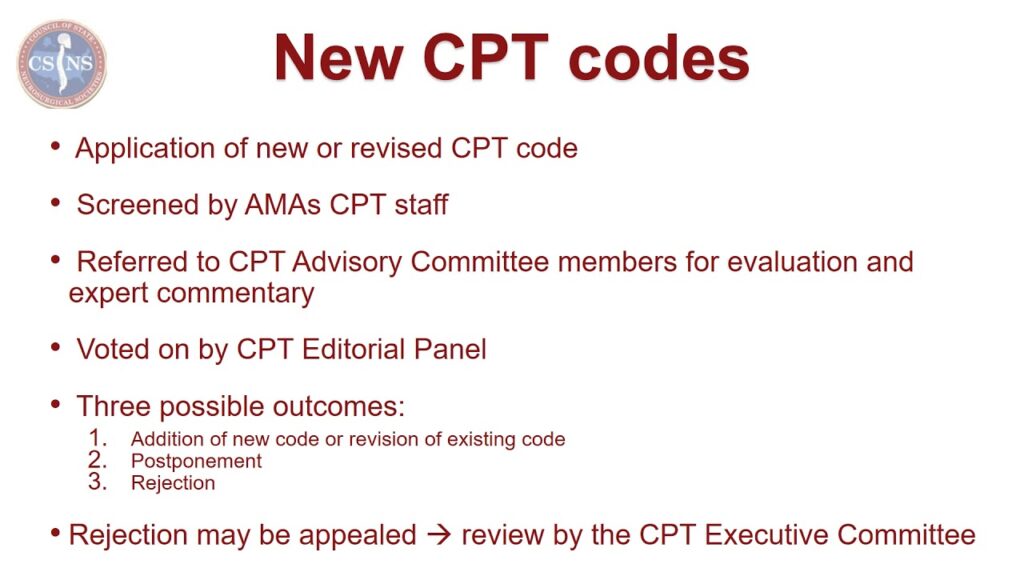
The review process typically involves the following stages:
- Initial Screening: The CPT Editorial Panel staff screens the application to ensure that it meets the basic requirements and completeness criteria.
- Expert Review: The application is then reviewed by subject matter experts who provide feedback on the clinical validity and utility of the procedure.
- Panel Deliberation: The CPT Editorial Panel discusses the application and considers the feedback from the expert reviewers.
- Public Comment: The panel may solicit public comments on the application to gather additional input from stakeholders.
- Final Decision: The CPT Editorial Panel makes a final decision on whether to approve or reject the application.
Understanding the Timeline New CPT Code Application
The timeline new CPT code application process can vary depending on the complexity of the procedure and the completeness of the application. However, a typical timeline is as follows:
- Application Submission: Applications are typically submitted by the deadline to be considered for the next annual update.
- Initial Review: Initial review by AMA staff takes approximately 1-2 months.
- Expert Review and Panel Deliberation: This phase can take several months, often 3-6 months, depending on the complexity and availability of experts.
- Public Comment Period: If deemed necessary, a public comment period may add another 1-2 months.
- Final Decision and Publication: Approved codes are typically published in the annual CPT code update, which is released in the fall and becomes effective on January 1 of the following year.
Therefore, the entire process from application submission to code publication can take 9-18 months or longer. Understanding this timeline new CPT code application allows applicants to plan accordingly.
Factors Affecting the CPT Code Application Timeline
Several factors can influence the timeline new CPT code application process:
- Completeness of the Application: Incomplete applications will be delayed or rejected. Ensure that all required information and documentation are included.
- Clinical Evidence: The strength and quality of the clinical evidence can significantly impact the review process. Robust evidence will expedite the review, while weak or lacking evidence can lead to delays or rejection.
- Complexity of the Procedure: Complex procedures may require more extensive review and deliberation, leading to a longer timeline.
- Controversy: If the procedure is controversial or raises ethical concerns, the review process may be prolonged.
- Panel Workload: The CPT Editorial Panel has a significant workload, and the timeline can be affected by the number of applications under review.
Strategies to Expedite the Application Process
While the timeline new CPT code application process can be lengthy, there are several strategies that applicants can employ to expedite the process:
- Prepare a Complete and Well-Organized Application: Ensure that all required information and documentation are included and presented in a clear and organized manner.
- Gather Robust Clinical Evidence: Invest in high-quality clinical research to support the safety and efficacy of the procedure.
- Engage with Stakeholders: Engage with relevant stakeholders, such as medical societies, payers, and regulatory agencies, to gather feedback and address any concerns.
- Seek Expert Guidance: Consider seeking guidance from coding experts or consultants who can provide valuable insights and assistance throughout the application process.
Post-Approval Considerations
Once a new CPT code is approved, the work is not yet complete. Several post-approval considerations should be addressed:
- Coding Education: Provide education and training to healthcare providers and coders on the proper use of the new code.
- Billing and Reimbursement: Work with payers to ensure that the new code is appropriately reimbursed.
- Monitoring and Evaluation: Monitor the utilization of the new code and evaluate its impact on healthcare outcomes and costs.
The Future of CPT Coding
The CPT coding system is continuously evolving to reflect the advancements in medical technology and healthcare delivery. As new technologies and procedures emerge, the need for new CPT codes will continue to grow. Understanding the timeline new CPT code application process and staying informed about the latest developments in CPT coding is essential for healthcare providers, administrators, and developers of new medical innovations.
The rise of telemedicine and digital health has also prompted the creation of new CPT codes to accurately represent these services. [See also: Telehealth Reimbursement Updates] The AMA continues to adapt the CPT coding system to meet the evolving needs of the healthcare industry.
Conclusion
The timeline new CPT code application process is a complex and rigorous undertaking. However, by understanding the key milestones, factors that influence the timeline, and strategies to expedite the process, applicants can increase their chances of success. Accurate and appropriate CPT coding is vital for reimbursement, data analysis, and compliance in the healthcare industry. Staying informed about the latest developments in CPT coding and engaging with relevant stakeholders is essential for navigating the complexities of medical coding.
The timeline new CPT code application requires patience and diligence. [See also: Understanding Medical Billing Codes] The process ensures that new medical procedures are properly documented and reimbursed, contributing to the advancement of healthcare.